The Enhanced Community Care (ECC) TransformationProgramme is of particular significance for the West of Ireland due to our ageing population and geographical makeup, write Tony Canavan and Breda Crehan-Roche, Chairs of the Joint Enhanced Community Care Governance Group.
In Community Healthcare West (CHW) and Saolta, the ECC programme has seen an investment of 372 staff into community teams across the region, developing services within four key areas for people living in the community.
These are the development of Integrated Care teams for Older Persons, Integrated Care teams for chronic disease management in Respiratory, Cardiology and Diabetes, the setting up of nine Community Healthcare Network Teams and further development of community diagnostics with direct GP access.
The approved posts are a combination of acute and community-based posts and include a number to further develop community-based diagnostics.
The benefits of the ECC Programme include supporting people to maintain a healthy lifestyle with the aim of keeping people in good health and providing health care closer to people’s home based on population needs assessment.
In Diabetes care it will facilitate patient access to dieticians and podiatry services in the community. For Cardiology, Rapid Access Diagnostic clinics and specialist cardiovascular clinics are among those that will be held in the community. For respiratory care Pulmonary Rehab clinics, breathlessness clinics and spirometry pathways are all being made available.
Primary Care and GP services will be delivered through multi-disciplinary and community specialist teams to people with complex needs and integration of community services, both voluntary and statutory, will improve community support to those who need it.
The health and wellbeing of the population as outlined in the Healthy Ireland Plan will be enhanced through partnership combining community supports and Health and Wellbeing initiatives. Reduction of lifestyle modifiable risk factors, the precursors of chronic illness, will be delivered through Health Promotion evidence based programmes e.g. Quit Smoking West Service.
Under the ECC Programme, discharge from acute hospitals is co-ordinated to ensure that people can return home to their own environment as soon as possible.
Under ECC, CHNs are being implemented across the country and are re-shaping how we deliver community healthcare services. These Networks support people to live more independently in their community by coordinating and integrating services.
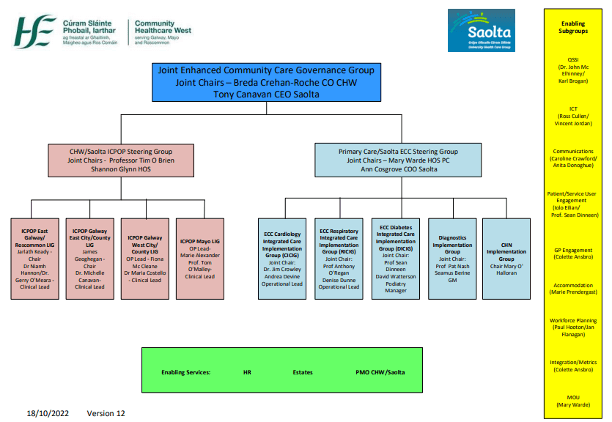
Governance
The governance structure for delivering ECC in Galway, Mayo and Roscommon is being led by Breda Crehan-Roche, Chief Officer, Community Healthcare West and Tony Canavan, Chief Executive Officer, Saolta University Health Care Group.


The programme steering group is chaired jointly by Ann Cosgrove, Chief Operating Officer, Saolta Group and Mary Warde, Head of Primary Care, CHW.


A number of multi-disciplinary Implementation Groups, for Cardiology, Respiratory and Diabetes, co-chaired by Integrated Care Consultants and operations leads are driving and supporting rollout of the clinical pathways. Several enabler Sub-groups have also been developed to support access across the ECC programme, including Diagnostics, Workforce Planning, ICT, Communications, Quality & Risk and Patient and GP Liaison. The Project Management Offices in CHW and Saolta are assisting developments.
In our Community Healthcare Organisation there are 9 CHNs:
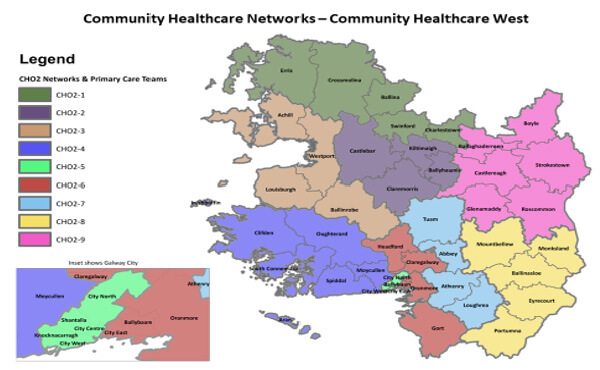
| Ambulatory Care Hub | Community Health Network Areas | Population |
| Galway City | West Galway, West Galway City, Central Galway and East Galway City | 156,693 |
| Ballinasloe | Tuam Athenry and Loughrea, East Galway and South Roscommon, North Roscommon and North East Galway | 158,025 |
| Castlebar | North Mayo, East Mayo, West Mayo | 130,638 |
Each CHN has a Network Manager, and a GP lead who supports the Network one day per week. They plan and prioritise network services, and improve communication and engagement between GPs and other Primary Care professionals within the Network. They also work with the Network Manager and Assistant Director of Public Health Nursing (ADPHN) to plan delivery of Network services on a population needs basis and support development and maintenance of relationships between GP’s and Primary Care professionals. The recruitment of our GP leads into the networks continues with full representation expected in Q2 of this year.
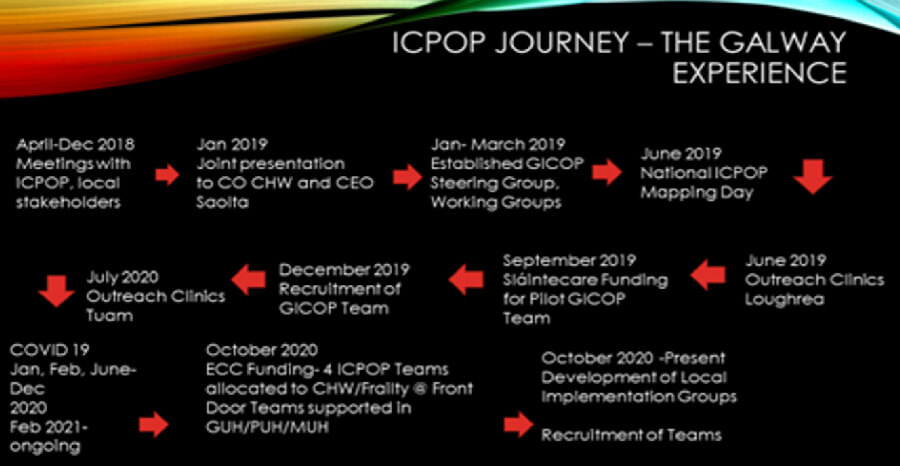
Integrated Care Programmes for Older People (ICPOP)
The Integrated Care Programmes for Older People and Chronic Disease has shown improved outcomes of older people who are frail and those with chronic disease, in terms of their diagnosis and ongoing care. Specialist multidisciplinary teams support networks and GPs and help link the care pathways between acute and community services.
CHW have been allocated 4 ICPOP Teams / 3 Frailty at the Front Door (FFD) Teams as part of the ECC Programme.
All four teams are now seeing patients either in their homes or in an outpatient community setting. Each team is seeing approximately 50 new clients a month as well as well as having approx. 100 interactions with clients already availing of the service. We would envisage that this will continue to grow as more staff are recruited, the referral sources expand and further outreach locations are commenced.
Each ICPOP team will consist of an Advanced Nurse Practitioner, Clinical Nurse Specialist x 2 (General) (Residential Unit Outreach), Consultant Physician in Geriatric Medicine, Dietitian, Grade IV, Grade VIII, Occupational Therapist, Occupational Therapy Assistant, Physiotherapist, Physiotherapy Assistant, Registrar, Senior Social Worker and Medical Speech & Language Therapist.
As part of the ECC Programme, three Frailty at the Front Door Teams are also being recruited in Mayo, Portiuncula and Galway University Hospitals. These teams will consist of a Clinical Nurse Specialist (General), Consultant Physician in Geriatric Medicine, Grade IV, Occupational Therapist, Physiotherapist, Physiotherapy Assistant and Registrar.
As a Sláintecare pilot, the Galway team was developed to provide Comprehensive Geriatric Assessment and Care for Older People in CHW in a community setting through the implementation of the ICPOP ‘10 Step Framework’. The multi-disciplinary team focus on developing integrated pathways for patients with Cognitive Impairment / Falls / Frailty. This initiative has been mainstreamed under the ECC umbrella and is providing great learning and support for the evolving ICPOP teams across the region.
Chronic Disease Hubs
Ambulatory Care for Chronic Disease Management focus on improving the experience of care for patients with COPD, Asthma, Type 2 Diabetes and Cardiovascular Disease.
This care is provided in an integrated fashion between GPs, Practice Nurses, Community Specialist Teams and Hospital Specialist Teams in designated community hubs. The hubs provide GPs and Practice Nurses with timely access to specialist assessment, diagnosis and treatment of patients in the community setting. These hubs also provide self-management, education and support services for patients.
In the West, three community specialist teams serving those with Chronic Disease including Respiratory, Diabetic and Cardiac teams are being established. Chronic Disease Management Hubs (CDM) will be developed in Castlebar, Co. Mayo and Knocknacarra and Ballinasloe in Co. Galway and interim accommodation arrangements are in place while we await this development.
An Operational Lead for each CDM team and other approved clinical staff have been appointed.
Separate implementation groups for Diabetes, Diagnostics, Respiratory and Cardiology meet regularly to address issues of recruitment, engagement and access for GPs and Practice Nurses. Implementation plans and standardised pathways for all groups have also been completed.
Integrated Information Communication Technology systems and tele-health will be important enablers.
Community Diagnostics
Enhanced access to Community Diagnostics, radiology, respiratory and cardiac diagnostics, for chronic disease and ICPOP teams as well as GP direct access will be available in the hubs and in outreach clinics in Primary Care settings. The group have identified equipment requirements and are tracking the recruitment of diagnostic posts to support service delivery. Progressing recruitment remains a key priority.
A subgroup has been established to specifically look at Phlebotomy / Laboratory needs to support the Programme.
Diabetes Integrated Care Implementation Group
Clinical Nurse Specialists (CNS) aligned to the Ballinasloe hub have commenced very successful fortnightly clinics. Both Dieticians and CNS’s have been running The Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (DESMOND) programmes across all three ambulatory care hubs, impacting significantly on waiting lists.
A validation of the waiting list in the Ballinasloe hub podiatry service was carried out last September which proved hugely successful. Work continues on the diabetic foot pathways with a focus on addressing service deficits on the acute hospital element of the pathway.
Multidisciplinary Team meetings are held twice a month with ongoing clinical support from Prof Sean Dinneen.
Cardiology Integrated Care Implementation Group (CICIG)
Clinical work has commenced with an initial focus on patients who have been recently hospitalised with heart failure. The HSE model of care for such patients includes a 12 week programme with review within 2 weeks of discharge.
Future goals include:
- Integration, reconfiguration and standardisation of hospital, general practice and community cardiology services, ensuring patients with cardiovascular disease receive timely, integrated and equitable access to a standardised programme of care.
- Rapid Access Diagnostic clinics (within one week of referral from primary care) for patients with suspected heart failure and atrial fibrillation with a one stop shop approach in terms of diagnostics, specialist assessment/therapeutic plan by IC Consultant and provision of education/self-management skills.
- Specialist Cardiovascular risk clinic with expansion of the Cardiac Rehabilitation programmes to provide all high risk patients (both primary and secondary prevention) with an evidence based CVD prevention/rehabilitation programme that comprehensively address their CV risk, including support from a Clinical Psychologist.
- Strong emphasis on audit of clinical and patient reported outcomes and service user engagement/feedback to provide high quality, effective, patient centred integrated care.
Respiratory Group
The Galway City Hub in association with local GP colleagues are linked with the national ICPCD team and are the pilot site for an elevation on a proof of concept pilot with technology company IQVIA. The pilot project is designed to provide the GP practice with on-site pharmacist led enhancement and augmentation of opportunistic case finding of patients with COPD. The aim is to provide impactful and helpful signposting to the GP and staff when seeking access to the range of services within the Galway City hub.
Pulmonary Rehab clinics are running in Westside, Oughterard, Clifden, Renmore, Gort, Headford, Ballinasloe with a pilot PR programme underway in the Mayo hub. A new diagnostic clinic, supporting Respiratory patients locally in Galway, is running in Merlin Park. This clinic ensures that patients can access a “one-stop shop” for diagnosis and have access to the consultant, a CNS, Physiotherapist and Respiratory Physiologist all on the same visit. The Galway City Hub has opened its GP Direct Access to Spirometry pathway where a Respiratory Physiologist is available to complete Spirometry on the patient and the results are reported on by the IC Respiratory Consultant and returned to the referring GP. This should assist in diagnostics moving into the community setting aligned to the hub and spoke model.
Health and Wellbeing
The appointment of a Health Promotion and Improvement Officer as part of the multidisciplinary team of each Chronic Disease Management Hub and in each of the associated Community Health Networks is a positive development. It promotes the prevention agenda to reduce the incidence of chronic illness and to prevent the development of co-morbidities among those who are already living with a chronic illness. Addressing the modifiable lifestyle risk factors e.g. smoking, nutrition, physical activity and mental health and wellbeing is key to improving population health and reducing the incidence of chronic illness over time.
Self-management support is a key workstream within Health and Well-being. Self-management support involves the provision of education and supportive interventions to increase a person’s knowledge, skills and confidence in managing their chronic health condition(s), and to support them in becoming an active partner in their own healthcare. Self-management support improves outcomes for patients – ranging from quality of life and clinical outcomes, to reduced healthcare utilisation including hospitalisation.
A Self-management Support (SMS) Co-ordinator is in post in CHW to support the implementation of the National Self-management Support Framework for adults living with chronic conditions. The SMS Co-ordinator is a member of each of the CHW ECC Implementation Groups – Cardiology, Diabetes, Respiratory and Patient Engagement. Supporting our service-users to self-manage is a core focus amongst our integrated care teams in CHW. The SMS Co-ordinator is supporting this process through the development and promotion of resources, which are designed to help our clinicians support self-management, and to help our service-users to engage with and manage their health conditions.
Saolta and CHW are committed to meaningful patient and service user engagement. Focusing on disease prevention and building healthy sustainable communities is a key part of the ECC programme. A ‘Better Together’ framework document is being developed in an effort to advise on how better engagement can take place with patients and staff members during the implementation of the programme. Better Together engagement days were held for patients and service users in June and October last year. Staff Workshops were held in October ’22 and January ‘23 focusing on patient and service user engagement with 62 staff in attendance.
Challenges in the Implementation Process
For the past 18 months while we have been working on the rollout of the ECC pathways there are a number of challenges that we are continuing to work through to develop optimal solutions.
One issue is securing the required level of accommodation to support service deliver in the various geographical locations.
Implementing ICT is also a challenge which we are working through, utilising existing systems in the acute hospital/community.
There are challenges in the recruitment of key specialist staff in particular in relation to diagnostics and dieticians. And ensuring a robust clinical governance structure is in place remains a priority.
Next Steps
Over the coming months we will continue our focus on the recruitment of key staff to support service delivery across all hubs in Galway, Mayo and Roscommon.
We will work with our ICT/OoCIO colleagues to configure and roll out existing ICT systems, in particular IPMS, Evolve and Healthlinks to enable the delivery of services and the communication required for patients, GPs and Hub staff.
We will continue developing relationships with our GP colleagues as we rollout the services.
In the ICPoP programme we will continue work on the frailty, falls and cognitive decline patient pathways.
Staff in CDMs and CHNs will be supported by management to undertake training towards the implementation of Making Every Contact Count (MECC) at a discipline and/or site level.
Importantly work has begun on identifying patients currently attending hospital outpatient services and who should be more appropriately attending the services that are being developed in the community hubs and our focus over the coming year will be on seeing more patients through the ECC Programme.
And finally within the networks the focus will be on the further implementation of an integrated approach to case management.

