The new programme will be delivered through dedicated multidisciplinary teams working in a network of Acute Medical Units, Acute Medical Assessment Units and Medical Assessment Units in three different levels of hospitals around the country, Prof. Shane O’Neill told the HMI Forum in Ardee, Maureen Browne reports.
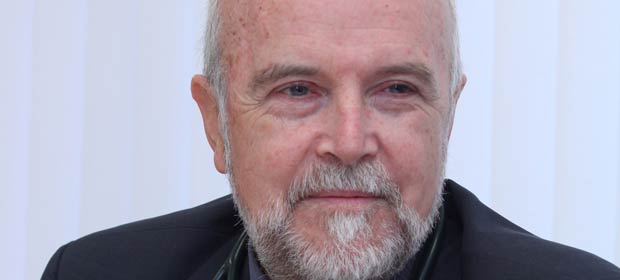
A new Acute Medicine Programme, which will be rolled out nationally next year, is set to transform patient care, according to Prof. Shane O’Neill, Clinical Director, Beaumont Hospital, Dublin and Joint Clinical Lead for the Programme with Prof. Gary Courtney of St. Lukes Hospital, Kilkenny.
He said that, under the new Programme, every patient will be seen by a senior doctor within one hour, the admission rate of medical patients will be reduced by 10 per cent without increasing 30 day readmission and very significant medical bed day savings will be generated.
He was speaking at the HMI Forum on “Leadership Challenges in a Changing Environment”, in the Regional Education Centre, at St. Brigid’s Hospital Complex in Ardee, Co. Louth.
The new programme will be delivered through dedicated multidisciplinary teams of doctors, nurses, therapists and medical social workers, in a network of new Acute Medical Units, Acute Medical Assessment Units and Medical Assessment Units in three different levels of hospitals around the country.
A Navigation Hub will allow Case Managers with senior clinical input to stream and re-stream patients referred by GPs and other services to the most appropriate pathways of care across the network.
Patients will be referred to the new units from primary care and from other sources including the hospital Emergency Departments. Decisions on whether patients should be admitted or discharged will be made within six hours of their arrival.
Model 4 hospitals
Acute Medical Units (AMU) will be based in Model 4 hospitals. Their primary function will be the immediate and early specialist management of adult patients, with a wide range of medical conditions who present to hospital.
Model 4 hospitals will have a 24-hour ED and a 24-hour AMU. The AMU will incorporate an Acute Medical Assessment Unit (AMAU) function and an adjacent medical short stay function. Where the AMAU is closed at night medical patients will be managed by the on-call Medical Team in the 24-hour ED.
Under the new Programme, every patient will be seen by a senior doctor within one hour
Patients presenting to the AMUs will be seen within one hour by a senior doctor, either a consultant, a senior registrar or a specialist registrar, who will have access to diagnosis and treatment facilities and who will decide if admission is necessary.
“The Unit will work on the basis of an acute floor, where diagnostic and treatment facilities will be aligned to it. This will be unlike the current situation where ED patients can be seen as an ED problem. We will have an acute medical unit, a coronary care unit, critical care, an interventional cardiology suite, an acute surgical assessment unit and a clinical decision unit,” he said.
AMUs will admit patients for a short period for acute treatment and/or observation where the estimated length of stay is less than 48 hours. Patients who require admission for longer than 48 hours will be moved from the AMU to a dedicated in-patient bed or ward.
Early warning score
A national Early Warning Score will be established to assist in the early detection of medical patients who deteriorate and to improve their outcome.
Similar type units but with key differences in their operational functions, will be established in Model 3 and Model 2 hospitals.
Model 3 hospitals will have Acute Medical Assessment Units (AMAUs) and Model 2 hospitals will have Medical Assessment Units (MAUs).
The Model 3 hospitals will have a 24-hour ED and, when the AMAU is not open on a continuous basis, all patients presenting with medical conditions will be managed by the Acute Medical team on-call in the ED, from two hours before the AMAU closes until it reopens.
A Navigation Hub will allow Case Managers with senior clinical input to stream and re-stream patients referred by GPs and other services
Model 2 hospitals will have an MAU where GP selected patients will be seen. These hospitals will admit undifferentiated acute medical in-patients. GPs will refer low-risk medical patients for assessment in the MAU during daytime hours. There will be a wide range of out-patient, diagnostic and day case surgery services provided.
Highest quality
There will be no MAU/AMAU/AMU in Model 1 hospitals. Model 1 hospitals will be Community/District Hospitals, with sub-acute in-patient beds.
Prof. O’Neill said that the Acute Medicine Programme has been established by the HSE Quality and Clinical Care Directorate and the Royal College of Physicians in Ireland. Its objective was to develop acute medicine services so that all medical patients would receive the highest quality of acute medical care and be assessed and managed in an effective and efficient manner.
It was envisaged that acute medicine would be developed as a specialty with acute medicine physicians heading up the programme.
Internationally Acute Medical Units have been shown to improve the efficiency of acute medical care, by increasing the proportion of patients discharged within 24 hours and by decreasing length of stay and overall medical bed day usage. A number of studies demonstrate that the introduction of an Acute Medical Unit (AMU), combining assessment and short-stay function, is associated with a decrease in hospital mortality for medical patients and no increase in re-admission rates.
The benefits of AMUs are derived through the efficient streaming of medical patients to a location where they can be seen without delay by a senior medical doctor who determines the clinical investigations and management they require and the most appropriate setting for their ongoing care. Advantages from the patient’s point of view are that extended waiting times are avoided and they have access to a senior clinician.

