The key challenges facing the Irish Health Services can be refocused into determining exactly how patient care delivery can be moved from being predominantly hospital centric to community centric and how best Chronic Disease Management delivery can be advanced in a comprehensive manner, Mr. Ian Carter, National Director of Acute Hospitals told the conference.

Speaking on “New Frontiers – Envisioning success for Irish Health Services” he said there is now general acceptance that the existing overall model of care delivery is both insufficient and not sustainable. With over focus on reactive episodic singular responses to acute / urgent patient requirements and generally not matching patient need particularly for those patients with chronic disease – approximately 75% of hospital patient activity.
There is as well a lack of integration between Hospitals, Primary Care and Social Care and by definition an absence of a robust integrated model of care. Within the current health service delivery paradigm the hospital remains the “last bastion of safety”.
A “big bang” vs “ incremental growth” vs “patch pilot” introduction should be agreed in advance
The current model results in the majority of acute hospitals operating at 100% full capacity, significant ED centred delays, less than optimal elective access, difficulty in discharging patients to the community following completion of acute episode of care and non sustainable cost growth.
Stepping back from these issues requirement to consider health needs from a population perspective and current focus in terms of service delivery orientation:
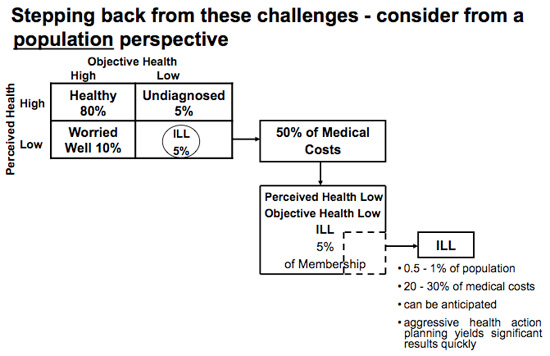
There is a requirement to consider Health Delivery needs from a population perspective that does not just focus on the 5% “ill”. This can be achieved through the development of a managed system of population care.
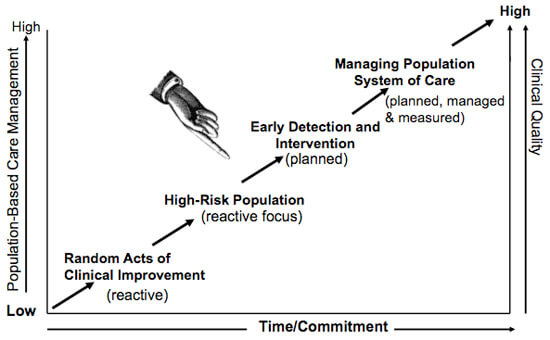
Mr. Carter said the progression framework must ensure the integration of the delivery systems of Primary Care, Social Care and Hospitals which would require both enhancement and investment and purposeful management. As well the framework should ensure resourcing is not competitive, performance metrics related to “clinical outcomes” are established – with necessary audit capability / capacity. In terms of implementation “big bang” vs “incremental growth” vs “patch pilot” introduction should be agreed in advance.

