
Ongoing staff support to minimise post-traumatic stress and improve well-being and continued strengthening of the Infection, Protection and Control (IPC) role and function, have been recommended in a landmark research into the management of COVID-19 in an Irish healthcare setting.
The research on “Service and care in a large, community long-term care facility,” carried out in the South Dublin based Older Persons Service, Leopardstown Park Hospital, found that a dedicated Isolation Unit, communication and decisive management response team were central to managing the virus in the 145 bed facility.

The aims of the study were to compare different Cohorts of residents that tested positive for COVID-19 and explore the nursing interventions when caring for a resident with COVID-19 detected result. It was also aimed to capture staff and residents’ experiences of COVID-19 management in a long- term care facility for older people.
This one-year project reviewed the management of COVID-19 in Leopardstown Park Hospital and through the vast source of data found evidence of challenging times but also accounts of creativity and connections. Urban location, use of isolation unit, nurses’ knowledge, quick adaption to a rapidly changing situation and professional experience were key in the management of COVID-19 infection in the hospital.
Situated in a densely populated urban suburb of Dublin, Leopardstown Park Hospital has a staff of 188 and cares for people with a broad range of complex needs. Its primary services include long term, supported accommodation, respite, rehabilitation and day-care services for those aged over eighteen years. Since the 1970s, LPH has welcomed non-military admissions and in 1979 the management and operation of the facility were transferred from the Leopardstown Park Hospital Trust to the Leopardstown Park Hospital Board under the Leopardstown Park Hospital (Establishment) Order, 1979.
LPH is considered home for its residents, and all levels of dependencies are cared for and include those who have dementia and/or are in need of end-of-life care.
The 135-page study, which was conducted over a twelve month period, in 2020/ 2021, presents a comprehensive review of the real-time management of COVID-19 during 2020-2021 from the perspective of both staff and residents.
Forty residents divided into three different cohorts tested positive for COVID-19 from April 2020 to February 2021. The largest cohort included in the study (55% of total residents) happened between January and March 2021. Overall, no clear relationship between residents’ coexisting conditions and symptoms as well as the COVID19 outcomes were found. Although residents were found to have high levels of frailty and vulnerability, this was not significant only to COVID-19 infection. Looking at the pre-existing conditions of the residents and the symptoms, as well as outcomes of the COVID-19 infection, no clear or significant correlation was found.
What became more significant was the care that was provided to those that tested positive for COVID-19. The use of isolation unit, rehabilitation programme and the role of the nurse were key factors that were important to have in place when caring for those with COVID-19. Care delivered to those with COVID-19 infection was dependent on a strong nurse knowledge and experience of older persons’ care along with the input of the interdisciplinary team of health care professionals. The COVID-19 management team, together with nursing management, became vital in the implementation of vast additional infection prevention and control measures. Measures such as social distancing, personal protective equipment and staff wellness checks entailed adaptation, not only for clinical staff but at all levels in the organisation. Measures that continued to be in place throughout 2021 and required rigorous auditing to maintain high standards. Strong leadership in LPH was key in managing the challenges and number of changes that were required.

The authors said there was no doubt about the major challenges COVID-19 had caused for long term care facilities for older people but there had also been opportunities to adapt practices and find solutions in a new ‘normal.’
The study found that the gardens became an escape from the everyday reminder of not being able to see family. Activities were provided outside when possible. Adaption of social activities did not mean that activities stopped. On the contrary, residents participated in activities that were new to them or they become more involved in the activities they had become used to. Some connection may have been lost with family members, particularly during strict lockdown measures, but the connection was found in other residents, staff and pets that visited.
The findings of the studyincluded:
- The central role nurses played in coordinating care.
- The use of a specific isolation unit as part of the outbreak management was a vital component.
- The importance of an experienced, knowledgeable, cohesive decisive management group was a major contributor to the successful management of the situation.
- Prompt symptom identification and initiation of the relevant protocols.
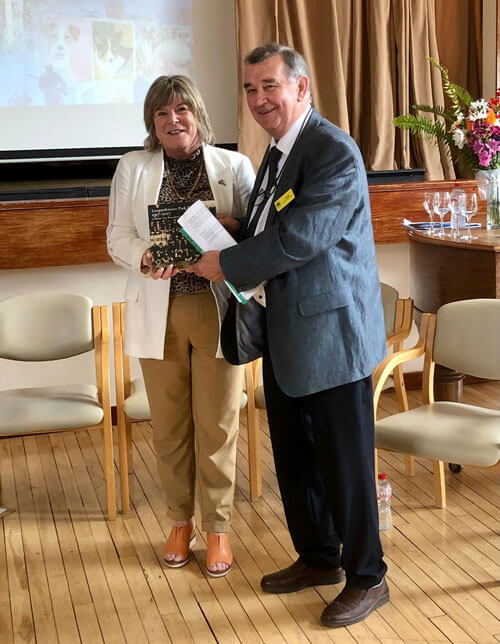
The research, co-authored by Mr. Adrian Ahern, Director of Nursing and Ms. Katja Savolainen, Research Nurse, was funded by the HSE through the regional Nursing and Midwifery Planning and Development Unit. Nursing, medical and HSCP team narrative notes, written and verbal accounts gathered through interview and minutes of meetings were extensively analysed, along with a literature review.
Speaking about the study, Ms. Ann Marie O’Grady, Chief Executive of Leopardstown Park Hospital said, “The emergence of COVID-19 had a fundamental and lasting effect on how we provide care to older people in Ireland and elsewhere across the world. Comprehensively assessing the issues that were encountered by those living and working in this environment while under sustained pressure as the virus rapidly emerged, was very important. Not just to be able to rightfully acknowledge what aspects of our approach could be strengthened, but to ensure that the appropriate practices are in place for future crisis scenarios.
“The COVID-19 Team have worked at very senior levels in many different organisations, dealing with all sorts of crisis situations. So, all of us had that, which included incredible operational and clinical strong nursing management including, critically, infection prevention and control expertise. So, we all had skills and tools within us.”
Mr. Adrian Ahern said, “The role, knowledge and expertise of our nursing staff was paramount. The impact of the pandemic on their own mental and physical wellbeing cannot be underestimated. Without their hard work and dedication, the COVID-19 virus could have had a far more detrimental impact for those for whom we care.”
Commenting on the importance of the research, Ms. Katja Savolainen said,“Studies such as this one are crucial as they provide perspective on one of the toughest challenges that have ever occurred in the modern, long-term care sector for older people, and allow us enhance our understanding.
There were no easy decisions during that period and these are not easy lessons to reflect on but there are valuable recommendations from this study that we and other similar facilities can consider during a public health pandemic in the future.”
Mr. Tony Morris, Chairperson of the Board of Managementsaid, “Although this project was limited to the experiences of those in Leopardstown Park, it reflects the resilience, and professionalism shown by so many across the Older Persons Service in working to reduce the impact of the virus.”
Leopardstown Park Hospital is registered by HIQA, funded by the HSE and recognised by the Nursing and Midwifery Board of Ireland (NMBI). It supports the training of undergraduate students from the Schools of Nursing in both University College Dublin and Trinity College Dublin. The Service also facilitates training in several other health-related disciplines including, Speech and Language Therapy, Dietetics, Pharmacy, Occupational Therapy and Physiotherapy.
The campus consists of a main building and one stand-alone premise known as the Clevis Unit which has 29 beds and cares for those who have low dependencies in line with the social care model. The main building is made up of four units – Enniskerry/Kiltiernan (21 beds) and Kilgobbin/Tibradden (20 beds). Units are multi occupancy collectively referred to as ‘Nightingale Units’. The two other long term care units, Glencullen and Glencree have 27 beds each. In addition to the long term care stay units, there are also Djouce, a 10-bed unit, which is predominately used for respite care, and Woodview which is used for rehabilitation.
*Adrian Ahern is the Director of Nursing/Person in Charge of Leopardstown Park Hospital, Dublin. He is a qualified psychiatric and general nurse and Addiction Counsellor. He has held a wide range of management roles in the HSE, including Local Administrator for Offaly Community Services, Administrator for St. Fintan’s Hospital Portlaoise and its community services, Manager, East Galway Mental Health and Older Peoples Services, General Manager of Mental Health Services including the regional CAMHS range of services and units, Complaints Officer under the Health Acts and Authorised Officer under the Mental Health Acts. He has lectured on Strategic Management at Athlone Institute of Technology, is a Council member of the Health Management Institute of Ireland and was the Irish nominee to the European Association of Health Managers, Mental Health Committee. In addition to his nursing qualifications he has a Diploma in Health Services Management, Certificate in Health Sector Economics, B.Sc. Econ., M.A. Health Care Management.
Katja Savolainen qualified as a nurse at Karolinska Institute in Sweden. In 2016 she completed her MSc in gerontological Nursing at Trinity College Dublin with a thesis on advance care planning in long-term care and is currently undertaking a Doctorate of Nursing in Trinity College Dublin where the research focus is on human rights of older people in long term care.

