The management of sepsis is a marker of the quality of acute care in the Irish health service. Sepsis accounts for 2 – 4% in-patient cases but contributes to 20% of in-hospital deaths.1 Early recognition and treatment can result in significant reductions in morbidity, mortality and bed days used, write Dr Vida Hamilton, National Sepsis Clinical Lead and Christina Doyle, Project Manager.

The presence of a sepsis quality improvement programme increases adherence to time-dependent care bundles and reduces mortality (OR 0.6).2 The aims of the National Clinical Sepsis Programme are to reduce mortality and enhance the quality of life in sepsis survivors by promoting early recognition, appropriate treatment and referral of patients with sepsis, thereby affording the maximum survival opportunity with reduced chronic sequelae. Secondary aims include reduction in length of stay.
Sepsis affects approximately 220 per 100,000 of the Irish population with an average mortality of 20%.
Epidemiology: Sepsis affects approximately 220 per 100,000 of the Irish population with an average mortality of 20%.1 International studies show that 70-80% of cases originate in the community and are admitted via the Emergency Department.3 Sepsis adversely affects Health-Related Quality of Life (HRQoL) in survivors4.
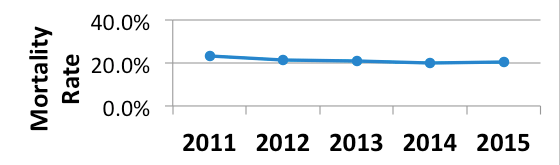
Problem: Sepsis is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection. Sepsis is a time-dependant medical emergency with a crude hospital mortality rate of 22.7% in Ireland (HIPE 2015). The introduction of time-dependant sepsis bundles aims to enhance recognition and treatment ultimately reducing mortality rates. This involves behaviour change to achieve the desired outcome, therefore requires buy-in as well as awareness, education and training. Initial rollout has been targeted at Emergency Departments (EDs) and inpatient settings in acute hospitals.
Targeted population: 70-80% of all sepsis cases are admitted from the community via the ED.3 Implementation of Sepsis bundles using a top-down, bottom–up approach in the acute setting identified roles and responsibilities for leadership teams and treating clinicians, and the formation of local hospital sepsis committees. An aligned approach to sepsis recognition and management is being developed through collaboration with specialist programmes, maternity, paediatrics, neonates, and primary care to develop a common language and approach to ensure consistency in care and communication.
55% of the population have heard of sepsis and most think heart attack is the highest killer despite it having a mortality rate of 6.4% compared to 20% for sepsis.
Methodology: the introduction of an integrated approach to sepsis recognition and management across the healthcare system services and specialties, addressing the issues which have been identified as contributing to patient morbidity and mortality.
- Failure to recognise the severity of illness
- Failure to recognise deterioration
- Failure to communicate effectively
- Failure to escalate care5
Step 1: National Clinical Guideline No. 6: Sepsis Management4
Published November 2014, NICE accredited March 2015. The accompanying implementation programme is aimed at patient detection and diagnosis and an initial treatment bundle that is titrated to individual needs and enables risk stratification and escalation and can be delivered by clinicians in all acute care settings.
Step 2: Education and Awareness
Medical and Nursing schools and Postgraduate bodies were contacted and asked to ensure that curriculae reflect the national guideline. A sepsis module is now included in the National Intern Training Programme (NITP). The e-learning programme was published on HSELand in October 2016 and is a mandatory component of the NITP starting July 2017.

Three National Summits have been hosted to date:
Hearts and Minds – aimed at Group and Hospital Leadership; Delegates were made aware of the new sepsis management guideline and asked to set up and support hospital sepsis committees for its implementation.
Start-up – aimed at Hospital Sepsis Committees with representatives from all acute hospitals present; early adopters discussed their implementation highlighting barriers and enablers.
At the Frontline – one year on representatives from hospitals around the county present their sepsis implementation work. Awards were given to Cavan General Hospital for best ED project, Limerick Regional for best oral presentation and Cork University Hospital for best poster.
At each summit sepsis survivors and bereaved family members spoke of their experiences of suboptimal care and loss. Evaluation was collected from delegates and collated and feedback and all summits were rated highly with the patients’ experiences being the consistently highest rated content.

Step 3: The Acute Hospital Sector – including Neonates, Paediatrics and Maternity. Pathways for time-dependent recognition and clinical decision support tools to facilitate accurate diagnosis and appropriate referral are being developed and put through PDSA cycles and pilots.
Step 4: The Pre-Hospital Sector – Paramedic pathway, GP pathway, Nursing Home and Prison Service, Ccommunity awareness. Tools are in development in collaboration with the relevant parties to support sepsis recognition and referral pathways in the Community.
Other information leaflets and other education aids for patient and healthcare professionals are available on our website www.hse.ie/sepsis. A national awareness survey demonstrates that 55% of the population have heard of sepsis and that most think heart attack is the highest killer despite it having a mortality rate of 6.4% compared to 20% for sepsis.
An integrated approach: the national approach to sepsis recognition and management is designed to work within the existing resources of the healthcare system and integrated with other relevant national programmes such as the:
- Cancer care programme
- NEWS
- IMEWS
- PEWS
- Anti-microbial stewardship committee.
- Communication and Handover
Step 5: Developing a reliable database for audit and feedback.
In collaboration with the Quality Improvement Programme and the Health Pricing Office, the national sepsis team developed a template for the measurement of the burden of sepsis in terms of incidence, mortality and healthcare usage for ongoing monitoring and feedback to service providers. To maximize the quality of the data the sepsis forms are designed to facilitate accurate documentation and coding and 7 sepsis workshops for coders were held with approximately 95% attendance to familiarise coders with the new forms and to increase knowledge and awareness.
The first National Sepsis Outcome Report was published on the December 8, 2016 at the first National Patient Safety Conference in Dublin Castle. Please click http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/SEPSIS-REPORTS.PDF to view the report. This report highlights the burden of sepsis to the community and healthcare system and provides baseline data for future monitoring of effectiveness of implementation and programme aims of mortality reduction and decreased healthcare usage over the five year roll-out. This report presents information on the burden of sepsis both to patients and the healthcare system and also the impact of sepsis form usage in the acute setting. The use of a standardised form improved the diagnosis and documentation of sepsis, resulted in a higher level of correct risk stratification and a higher rate of antimicrobials administered within the first hour (74.5% with form versus 46% without sepsis form).
Conclusion
Sepsis incidence is impacted by age and co-morbidities, in the context of an ageing population, it can be anticipated that the incidence will increase. This will lead to an increased burden to the acute sector that can be modified by compliance with the National Guideline. Similarily, the impact of sequelae in survivors such as increased healthcare usage, reduced health-related quality of life, and decreased productivity can be ameliorated by early diagnosis and appropriate care.
References
- Health Service Executive, 2016. National Sepsis Outcome Report 2011 -2015 http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/SEPSIS-REPORTS.PDF
- Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Rhodes et al; CCM, March 2017, Vol 45, No.3, 486-552.
- CDC Vital Signs, 2016
- Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010 Oct 27;304(16):1787-94. Iwashyna TJ et al.
- Investigation into the safety, quality and standards of services provided by the Health Service Executive to patients, including pregnant women, at risk of clinical deterioration, including those provided in University Hospital Galway, and as reflected in the care and treatment provided to Savita Halappanavar. HIQA, October, 2013
- National Guideline No. 6: Sepsis Management, www.hse.ie/sepsis

