The HSE is a transparent and accountable organisation with performance monitoring and management arrangements in place to focus on driving operational performance improvements and also to deal with under performance and where the health providers fail to meet their targets, Ms. Laverne McGuinness, HSE Deputy Director General told a meeting of the HMI Dublin Mid Leinster Regional Meeting in the Dublin Dental Hospital last Thursday evening.

Speaking on “Planning and Accountability in the HSE,” she said the HSE is a very transparent organisation with its corporate plan, service plan, and performance and monitoring reports all published and available on line.
The HSE is very publicly accountable to the Oireachtas and frequently appeared before the Oireachtas Joint Committee on Health and the Public Accounts Committee.
In respect of some specific service targets there is a zero tolerance for service providers who fail in serious areas to deliver the safe and quality patient care required to meet the targets. For example, every patient who requires an urgent colonoscopy is expected to be seen within 28 days and there is a zero tolerance in place for failure to meet this target.
Ms. McGuinness said the HSE has a vision for the health service which is set out in its Corporate Plan. The Vision being “A healthier Ireland with a high quality health service valued by all” is translated into goals and actions. The actions to be addressed each year are set out in the Annual Service Plan. The HSE measures what gets done each month and publishes the results in the Monthly Performance Report using the Balanced Scorecard approach and a Performance Accountability Framework.
A key focus for 2015 and 2016 is in strengthening governance and accountability arrangements. A new National Performance Oversight Group is in place for 2015 and each National Director responsible for service delivery attends and gives an account of their service performance to the oversight group each month. Underperformance in service areas is discussed and plans to address the deficits are sought. Whilst a lot of work has been done on the Accountability Framework in 2015 further work is on-going to develop the the framework and in particular the intervention and support processes.
“The Accountability Framework sets out the Performance Management Process for the Health Services and how senior managers are held to account for performance grouped across four key areas – Access, Quality, Finance and People. The overall purpose is to improve service performance and quality of the services for our patients and our service users.

“We have introduced new formal Performance Agreements between the Director General and National Directors with explicit arrangements for escalating areas of underperformance and with a range of interventions.”
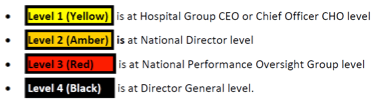
The Deputy Director General said that where service providers do not meet some of the key targets identified there is a four point escalation framework in place.
The characteristics of issues in the Red Escalations category are:
- A serious concern to service delivery, quality and safety of care
- Frequency or persistence of problems appear to exceed that which can be dealt with through routine arrangements
- Failure to maintain an agreed improvement trajectory following Amber Escalation or an issue of serious concern in its own right.
Supports available include:
- Partnering with a high performer as a source of support and advice
- Formal improvement plan
- Increased frequency of engagement with National Director
Interventions at this level include:
- Appointment of an Improvement lead
- Full Governance Review – diagnostic report
- Special meetings between NPOG and HG or CHO management team
Sanctions include:
- Performance Notice
- Differentiated approach to financial sanctions including restrictions on recruitment
She gave some examples of improvements which have been made from the level of focus and scrutiny placed on underperformance under the Escalation and Intervention Framework. These included:
- Child & Adolescent Mental Health patients waiting >12 months for first appointment – month on month improvement in number of long waiters.
- Process improvements in Rapid Access Cancer Clinics – Lung, Prostate and Radiotherapy.
- Patients waiting > 4 weeks for urgent colonoscopy.
- Routine colonoscopy → review of clinical needs being carried out to drive improvement in performance.
Ms. McGuiness said that the responses of patients and clients to the HSE Behaviours and Attitude survey on their experience with the services over the previous 12 months varied depending on their actual experience”.
Most of the patients reported they had had a good experience. This should be seen in the context of the broad range of services provided by the HSE – 1.4 million patients received inpatient or day case treatment each year, 3.2 million attended a hospital outpatient department each year and 1.2 million attended emergency departments each year.
Of those who had been to a hospital for a procedure, 97% reported an excellent or good experience, 92% reported an excellent or good experience at the local health centre while 62% reported an excellent or good experience at the A&E department.
The levels of satisfaction and patient experience with the service is a tribute to all the staff involved in delivering them and we need to acknowledge the excellent job that our staff do. However we also need to acknowledge when we do not do a good job and when we let the patient down.
She said examples of poor experience were what had happened in Portlaoise and in Aras Attracta.
“The lack of compassion, dignity, respect, and the lack of kindness experienced by patients and clients in these instances was shocking and deeply upsetting for patients and relatives, and for all of us in the HSE,” said Ms. McGuinness.
“These instances have shown an uncaring culture, which is the opposite of our Values which are Care, Compassion, Trust and Learning. Whilst improvements have and continue to be made in our services we need to do better.”
She said the HSE’s ambition for the Health Service over the next three years is set out in its Corporate Plan. Its vision is for a “healthier Ireland with a high quality service valued by all.”
The Corporate Plan has five goals:
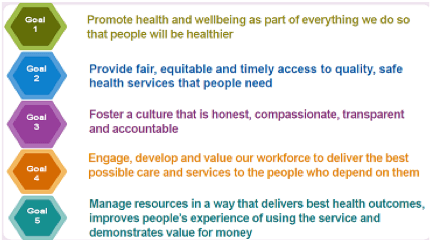
“Underpinning each of these goals are our values of Care, Compassion, Trust and Learning.
Progress on the delivery of these five goals, actions to deliver them and the measures of success will be set out each year in the Annual Service Plan. Delivery will take place though the seven Hospital Groups and nine Community Healthcare Organisations
Ms. McGuinness said there are a number of key areas of focus for the coming year including:
- Health Service Reform
- Quality and Patient Safety
- Changing the Culture and empowering staff
- User and Patient at the centre of our services
- National clinical programmes and integrated care programmes- reflecting national policies including the Healthy Ireland Framework, Knowledge and Information Strategy etc
- Reflecting Ministerial Priorities and DoH Statement of Strategy
- Establish and develop Hospital Groups, including National Children’s Hospital
- Establish and develop Community Healthcare Organisations
- Develop clinically led Integrated Models of Care
- Develop and implement the new finance operating model
- Develop and implement activity-based funding
- Reform of Human Resource Management
- National Ambulance Service
- ICT reform in line with the eHealth Strategy

