The need to implement a radical change programme necessary to deliver a quality care in the rapidly constraining fiscal environment of 2007 – 2014 was paramount and resulted in significantly increased efficiency and performance in Cork University Hospital, writes Mr. Tony McNamara, Chief Executive Officer, Cork University Hospital.

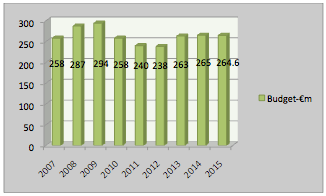
As a direct consequence of a catastrophic economic situation, annual expenditure on the Irish health system contracted by over €2.0bn (c. 15%) in 2014 relative to 2007. The annual incremental reduction in the intervening years is reflected in the annual resourcing of Cork University Hospital (the Hospital), a 750 bed multi-specialty teaching hospital and is set out in Figure 1.
The resultant need to implement a radical change programme necessary to deliver a quality care in a rapidly constraining fiscal environment was paramount and resulted in significantly increased efficiency and performance in the Hospital. The manner in which this was achieved and some of the changes that were implemented are presented in this article.
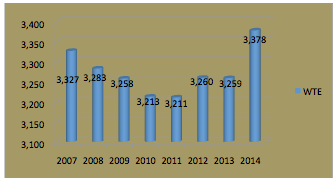
In what is a staff intensive environment, pay costs account for over 70% of the annual budget of the Hospital and Figure 2 represents the trend in staff numbers employed in the period 2007 – 2014.
Of necessity much of the focus in implementing the change programme related to initiatives designed to reduce pay expenditure and to deliver services differently and creatively. In essence the Hospital had to implement enormous change at a rapidly accelerated rate, a challenge that differentiates this process from others and which offers learning for other similar change programmes in other countries.
Government pay policy incorporating a moratorium on the employment of staff, pay reductions and increased taxes, created a climate of conflict and an adversarial environment in which the implementation of change was ever more difficult.
Government pay policy incorporating a moratorium on the employment of staff, pay reductions and increased taxes, created a climate of conflict and an adversarial environment in which the implementation of change was ever more difficult. The agreement reached between unions and the Government in 2010 termed the “Croke Park Agreement” incorporated provisions that facilitated change in return for employer undertakings that pay would not be further reduced. This Agreement and a subsequent similar agreement reached in 2013 provided the basis for the implementation of changes in work practice, revised staffing arrangements and changes to skill mix creating the environment for a more cost efficient service.
What were the key changes that leadership in the hospital made in response to this new set of circumstances? These can be summarised into a combination of voluntary redundancies, major reorganisation of services including a total change in the delivery of clerical administrative functions involving over 85 staff, redeployment of staff to critical functions, outsourcing of some processes and reallocation of management functions. This combination of changes was not easy but staff demonstrated a willingness and capability to effect these changes particularly so in the context of severe changes in their terms of employment.
During this period, a very challenging change programme was being implemented involving a radical reorganisation of services between hospitals in the greater Cork region. This followed a report recommending changes in the service profile of hospitals coupled with the Small Hospitals Framework, such that Cork University Hospital was to become the trauma and cancer centre for the region. These changes were effected with an insufficient transfer of resources to the Hospital thereby creating greater pressure to not only implement these changes but to meet challenging key performance indicators in respect of the cancer programme and national performance targets. Indeed during the period 2009 – 2013 the Hospital was in a constant state of revolutionary change with additional services and demands on an ever reducing staff numbers.
This may provide learning points for other countries facing similar economic challenges with reductions in healthcare funding.
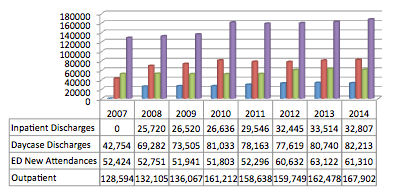
These changes in service configuration resulted in significant upward adjustments to activity and consequently put increased stress on an already stressed system. The impact on activity levels is represented in Figure 3.
It is to the credit of staff that the collective response was to implement changes in work practices and service delivery that enabled the hospital not only meet these challenges but to improve performance in respect of patient flow, waiting lists and departmental efficiency. In this regard to use of Lean Management and Six Sigma techniques in departments such as the Emergency Department, Theatres and Bed Management helped reduce redundancies in the system and improve the quality of service for patients.
Work on this change management and quality improvement programme is progressing with the implementation of national care programmes which have collectively helped to provide direction to service and process changes and which continue to contribute to improved efficiency and quality of service.
In conclusion, despite very traumatic changes to the terms and conditions of staff, very radical change has been embraced by staff and this may provide learning points for other countries facing similar economic challenges with reductions in healthcare funding.

